Incontinence surgery, also known as urinary incontinence surgery, refers to a group of surgical procedures designed to treat urinary incontinence—a condition characterized by the involuntary loss of urine. These surgeries aim to improve or restore bladder control.
Incontinence surgery is typically performed when conservative treatments, such as lifestyle modifications, pelvic floor exercises, and medications, have proven ineffective in managing urinary incontinence. The exact timing of the surgery depends on the type and severity of incontinence and the patient's preferences.
The primary purposes of incontinence surgery are:
To alleviate or eliminate urinary incontinence and regain control over bladder function.
To improve the patient's overall quality of life by addressing the physical and emotional impact of incontinence.
There are various surgical procedures to treat urinary incontinence, and the choice of procedure depends on the type and cause of incontinence. Common procedures include:
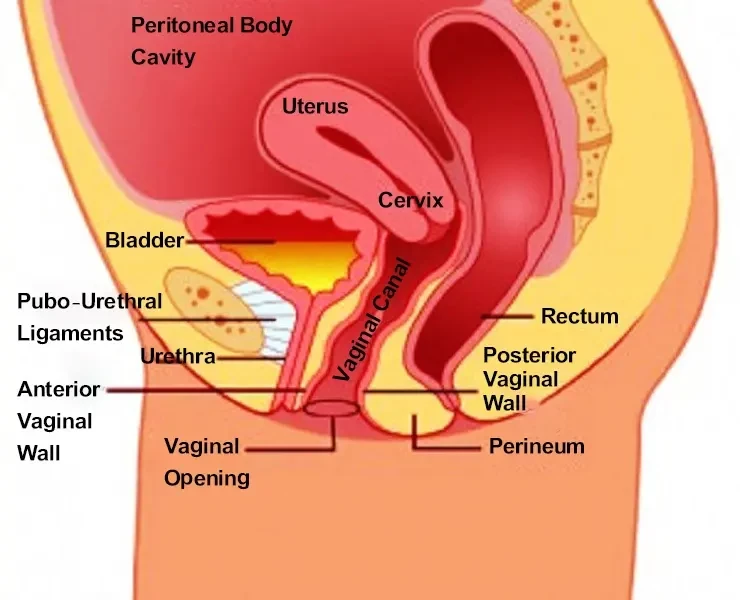
The placement of a supportive "sling" under the urethra or bladder neck to provide support and improve closure during moments of stress (e.g., coughing or sneezing).
The suspension of the bladder neck and urethra to reposition and stabilize them.
Implantation of a device that mimics the function of the urinary sphincter, allowing the patient to control urine flow.
The injection of a substance around the urethra to increase resistance and prevent urine leakage.
Implantation of a device that sends electrical impulses to the nerves controlling bladder function to improve control.
The choice of anesthesia (general or regional) depends on the specific procedure and patient factors.
Incisions vary depending on the surgical approach. Some procedures are minimally invasive, requiring small incisions, while others may involve larger incisions and some procedures are done through vagina.
Surgical instruments may include scopes, sutures, sling materials, or specialized devices for implantation (e.g., AUS).
The length of incontinence surgery varies based on the chosen procedure but often ranges from 30 minutes to a few hours.
Monitoring equipment, including ECG and blood pressure monitors, is used to ensure the patient's safety during surgery.
Potential complications of incontinence surgery may include:
Expected outcomes depend on the type of incontinence and the success of the surgical procedure. Most patients experience significant improvement in bladder control following surgery.
– Alternatives to Surgery
Before considering surgery, conservative treatments such as pelvic floor exercises, lifestyle modifications, and medications should be explored. These may be effective for some individuals with incontinence.
– Scarring
The extent and visibility of scarring depend on the type of surgery. Minimally invasive procedures often result in smaller, less noticeable scars.
Post-operative care includes:
– Hospital Stay
The length of hospital stay varies but is often short for minimally invasive procedures. Some procedures may be performed as outpatient surgeries.
Recovery time depends on the type of surgery and individual factors but generally follows this pattern:


 Whatsapp Now
Whatsapp Now +918106688026
+918106688026